June 13, 2022
Study explores the promising but still puzzling field of stem cell therapy for painful joint injuries

An interdisciplinary group of researchers from across the University of Calgary campus has received two years of funding from the New Frontiers in Research Fund (NFRF) to explore novel stem cell therapies to treat challenging joint injuries that can lead to chronic pain in horses and humans.
Joint injuries involving both soft tissue and cartilage damage are common in both equine and human athletes, and poor healing can lead to chronic joint pain. Researchers are studying how stem cell therapy may help with healing.
“Our equine athletes are no different (than humans), and this opportunity to put our minds together to investigate treating these challenging injuries is really exciting for both veterinary and human medicine,” says Dr. Holly Sparks, DVM, PhD'19, assistant professor of large animal surgery in the Faculty of Veterinary Medicine (UCVM) and Canada Research Chair (Tier II) in Equine Regenerative Medicine.
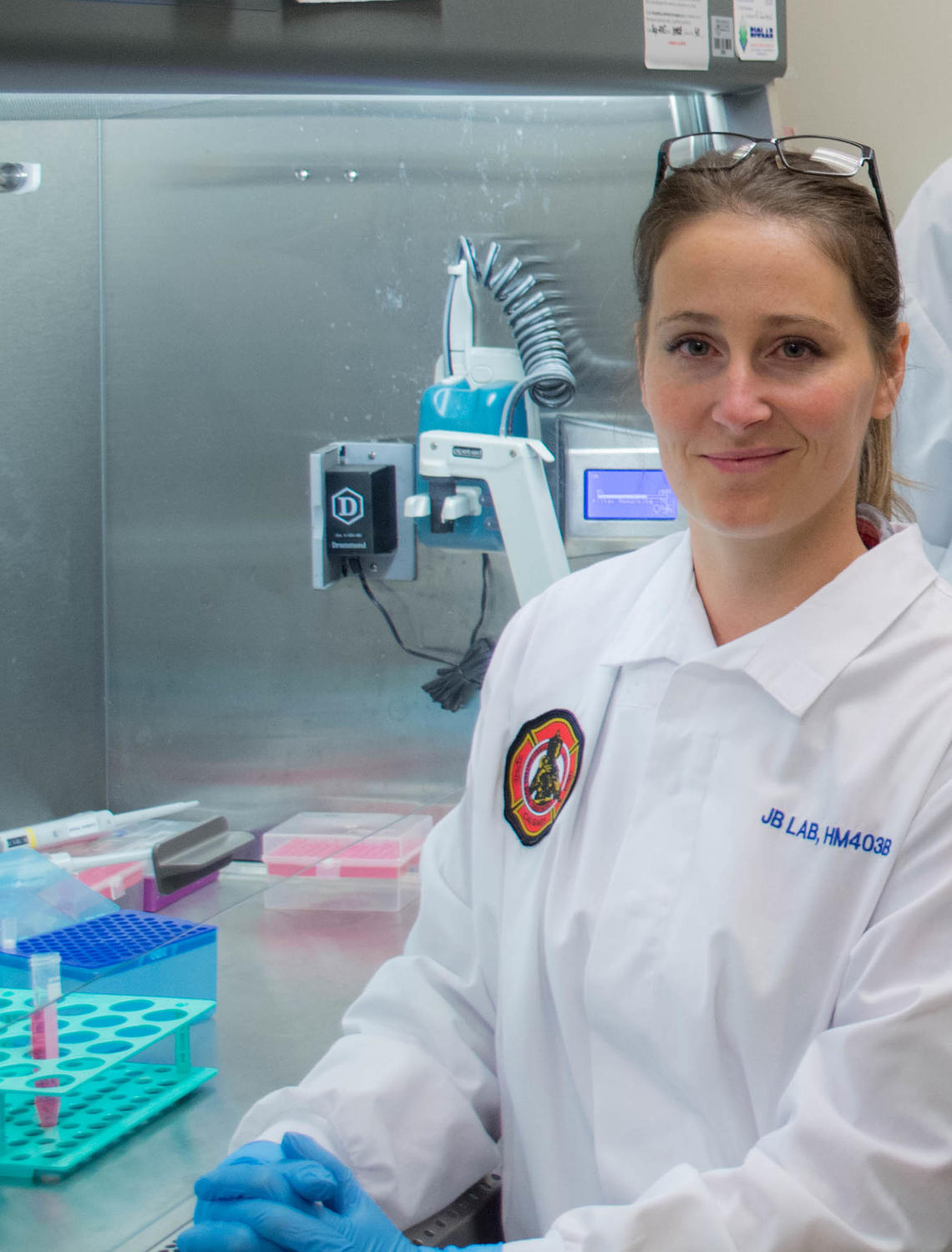
Dr. Holly Sparks, DVM, PhD'19 – a large-animal surgeon and regenerative medicine researcher – is involved in a collaborative project investigating stem cell-based approaches to treating joint injuries in veterinary and human medicine.
Rahil Tarique
“We’re looking at utilizing regenerative-medicine approaches to treat these injuries early, in a way that will hopefully encourage more functional healing in the short term and reduce joint pain in the long term,” says Sparks.
Not a single stem cell therapy approved for use in North America — yet
While there is a lot of promise for stem cell therapies, and no shortage of pre-clinical studies around the world, not one stem-cell therapy — for humans or animals — has yet been approved for use in North America.
“There has been a disproportionately large amount of work done in this area, but we're no closer to an answer because there's so much variability in how people conduct this research,” says Dr. Roman Krawetz, PhD, an associate professor specializing in stem cells and tissue engineering at the Cumming School of Medicine (CSM), member of the McCaig Institute for Bone and Joint Health at the CSM, and Canada Research Chair (Tier II) in Bone and Joint Stem Cell Biology.
The collaborative research team also includes Dr. Brent Edwards, PhD, associate professor in the Faculty of Kinesiology, who researches biomechanics and musculoskeletal injuries; Dr. Mike Scott, DVM, associate professor at UCVM and surgeon at Moore Equine in Calgary; and Dr. Arindom Sen, BSc'91, MSc'98, PhD'03, a professor in the Schulich School of Engineering who studies how to scale up production of stem cells. “This interdisciplinary team approach is really the key to this work, and the chance to work together on this is a really exciting opportunity,” says Sparks.

Dr. Roman Krawetz, PhD, an associate professor in stem cells and tissue engineering, says, while there’s been a large amount of work done in stem cell therapy research, “we’re no closer to an answer.”
Supplied by Roman Krawetz
The researchers will apply the “highest possible standards” in consistently producing and applying stem cells for the specific application to the stifle joint, or the equine equivalent of the human knee. As well as strict quality control on how stem cells are grown, collected and manipulated, the team has the clinical knowledge to assess the outcomes.
Study aims to shed light on evolving field of stem cell therapy
“Did this have any benefit? And if so, where? Did it regrow cartilage? Did it reduce inflammation? Did it reduce pain?” says Krawetz. “Whatever answer we get is going to be important to the field. If we can show that it's beneficial, great. If we show that it's not beneficial, I think that that's equally important.”
The research will not only help guide veterinarians and horse-owners managing these types of injuries, but will also add significantly to the emerging body of knowledge around stem cells. “While cell-based therapy shows considerable promise for treating musculoskeletal injuries like those studied here, there's still a lot to be learned about how stem cell therapy may work,” says Sparks. “Hopefully, we can shed some light on that with this project.”
Dr. Roman Krawetz, PhD, is an associate professor at the departments of Cell Biology & Anatomy, and Surgery at the Cumming School of Medicine (CSM) and a member of the McCaig Institute for Bone and Joint Health at the CSM. He is the Canada Research Chair (Tier II) in Bone and Joint Stem Cell Biology.
Dr. William Brent Edwards, PhD, is an associate professor in the Faculty of Kinesiology and in the Department of Clinical Neurosciences at the CSM. He is also a member of the McCaig Institute.
Dr. Arindom Sen, BSc'91, MSc'98, PhD'03, is a professor in Chemical & Petroleum Engineering with the Schulich School of Engineering and a member of the McCaig Institute.
Dr. Holly Sparks, DVM, PhD'19, is an assistant professor in Veterinary Clinical and Diagnostic Sciences, Faculty of Veterinary Medicine, and a member of the McCaig Institute. She is Canada Research Chair (Tier II) in Equine Regenerative Medicine.




